The contagion illusion: How toxins mimic infection and challenge modern medicine
11/25/2025 / By Willow Tohi
- A growing body of evidence suggests many disease symptoms are the body’s response to toxins, not infections from viruses.
- Cells under chemical stress release extracellular vesicles (exosomes), which are nearly identical in size and structure to viruses.
- These exosomes carry distress signals that can trigger illness in other parts of the body, creating a systemic response to a localized toxin.
- Historical and modern outbreaks, like St. Anthony’s Fire and the 2019 EVALI crisis, show how toxic exposures can mimic contagious diseases.
- The difficulty in distinguishing between viruses and exosomes challenges the accuracy of some diagnostic tests and our fundamental understanding of disease.
What if the fevers, coughs and inflammation we blame on viruses are not signs of infection, but rather our body’s sophisticated response to poisoning? A growing body of scientific evidence is challenging a cornerstone of modern medicine, suggesting that many illnesses historically attributed to contagious microbes may instead be the result of exposure to environmental toxins. This paradigm shift centers on tiny particles called extracellular vesicles, which are so similar to viruses that they can create the illusion of contagion, forcing a re-examination of how we diagnose and treat disease.
When your cells sound the alarm
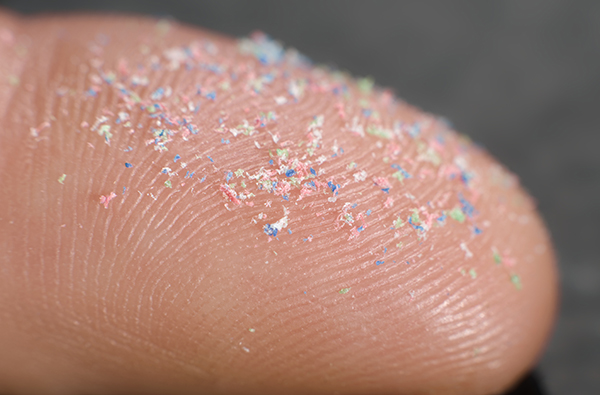
The mechanism behind this phenomenon involves extracellular vesicles (EVs), particularly exosomes. These are nano-sized packets that cells release to communicate with each other. Under normal, healthy conditions, they are essential for immune coordination and healing. However, when cells are stressed by toxins—including pharmaceutical drugs, pesticides, heavy metals, or air pollutants—they release a storm of these vesicles loaded with a very different cargo: distress signals.
These stress-laden exosomes package the molecular signature of injury, such as inflammatory chemicals and death signals, and ship them throughout the body. When a healthy cell absorbs one of these packets, it can respond as if it, too, has been directly poisoned, activating the same inflammatory and injury programs. This means a toxin damaging a single organ, like the liver, can trigger a whole-body crisis through this cellular messaging system, without the original toxin ever reaching other organs.
Historical and modern outbreaks re-examined
This mechanism provides a new lens through which to view disease clusters that have long been assumed to be infectious. In medieval Europe, waves of “St. Anthony’s Fire” caused burning pain, gangrene and death, sweeping through villages in a pattern that suggested contagion. Centuries later, the cause was identified as ergot, a fungus that contaminated rye grain. The entire community fell ill not from person-to-person spread, but from a shared toxic exposure, with the synchronized timing creating the appearance of an epidemic.
A strikingly similar pattern emerged in 2019 with the EVALI (E-cigarette or Vaping product use-Associated Lung Injury) outbreak in the United States. Thousands of young people were hospitalized with severe respiratory symptoms that doctors initially diagnosed as a mysterious viral pneumonia. The CDC investigation, however, revealed the culprit was not a virus but vitamin E acetate, a chemical adulterant in vaping products. The toxin caused lung damage that mimicked infection so perfectly that it fooled clinicians, and because friends shared tainted cartridges, the illness appeared to spread through social networks.
The diagnostic dilemma: Virus or exosome?
A primary reason this confusion persists is the remarkable biophysical similarity between viruses and exosomes. They are virtually identical in size, shape and density, making them difficult to separate in a laboratory. Under an electron microscope, a virologist may struggle to distinguish a coronavirus from an exosome. Both are encased in a lipid membrane and carry nucleic acids and proteins.
This overlap creates significant diagnostic challenges. PCR tests designed to detect viral genetic material can potentially amplify sequences found within exosomes, which may carry fragmented or dormant viral code as part of the body’s immune response. This raises questions about the specificity of tests that rely solely on detecting a piece of genetic code, as they may be identifying a signal of the body’s distress rather than a replicating pathogenic virus.
Rethinking the nature of illness
The implications of this research are profound, suggesting that a portion of what we call “viral illness” may be the body’s adaptive, though sometimes overwhelming, response to chemical injury. The “Xenogen Hypothesis” posits that particles labeled as viruses are often the body’s own exosomes, deployed to manage and adapt to environmental threats like toxins and electromagnetic stress. This framework views symptoms not as the attack of an external invader, but as the visible manifestation of the body’s intense effort to heal and detoxify.
A call for a more nuanced approach to health
This emerging science does not dismiss the reality of infectious pathogens but argues for a more nuanced understanding of disease etiology. It suggests that public health must place a greater emphasis on reducing widespread chemical exposures and that medical diagnostics need to evolve to better distinguish between true infection and toxin-induced illness. By recognizing the body’s sophisticated communication system and its response to environmental poison, we may open the door to more effective, less toxic approaches to healing that support the body’s innate intelligence rather than merely suppressing its symptoms.
Sources for this article include:
Submit a correction >>
Tagged Under:
This article may contain statements that reflect the opinion of the author